The Problem: Many immigrants are denied health care, leaving moms and babies at risk
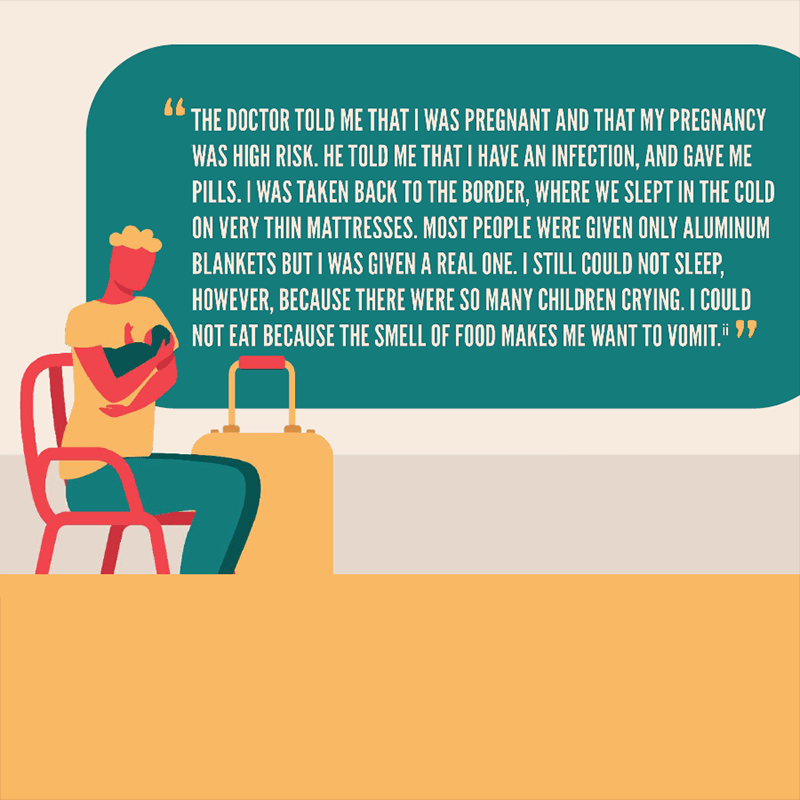
Every day in the United States, immigrants contend with xenophobia, racism, and intense individual and community-level trauma, whether they have legal documentation or not. This mistreatment is rooted in historical and ongoing oppression and discrimination, including forced separation from their families at the border, inhumane conditions in immigration detention facilities, denial of access to services even for those legally present, and other anti-immigrant policies. This maltreatment significantly increases the risk of poor mental and physical health for immigrant people and their families, including for pregnant people and infants.*
 Even so, immigrants are systematically denied health care. A constellation of discriminatory laws and policies leave limited affordable health care options for immigrants, thereby compounding the harm they experience. Health care is a basic human right, and it is crucial that we ensure access to high quality, language-accessible, and culturally congruent health care services for all people in the United States, including immigrants, to ensure their health, well-being, and dignity.
Even so, immigrants are systematically denied health care. A constellation of discriminatory laws and policies leave limited affordable health care options for immigrants, thereby compounding the harm they experience. Health care is a basic human right, and it is crucial that we ensure access to high quality, language-accessible, and culturally congruent health care services for all people in the United States, including immigrants, to ensure their health, well-being, and dignity.
Immigrant people are less likely to have access to health insurance compared to native-born people. While slightly more than half of U.S. families obtain health insurance via their employer, many immigrants are segregated into jobs and industries that are less likely to offer employer-sponsored coverage. Moreover, immigrant workers are also more likely to have lower incomes and are often priced out of insurance.
Documented immigrants may become eligible for coverage through Medicaid or the Children’s Health Insurance Program (CHIP), but many states still require a five-year waiting period after being considered “legally present” in the country. However, some who are eligible still hesitate to use these benefits because they fear that they or a family member will be subsequently denied permanent residency (green cards) under the so-called “public charge” standard. Undocumented immigrants are prohibited from obtaining federally funded health care through Medicaid, CHIP, or the Affordable Care Act marketplaces, with the exception of emergency Medicaid, and then only to cover stabilization. As a result, almost half of undocumented immigrants and 25 percent of lawfully present immigrants are uninsured and generally cannot afford the high cost of care, compared to only 9 percent of citizens.
Whether insured or not, other obstacles stand in the way of immigrants accessing care. These include, but are not limited to, the inability to cover cost-sharing, the complexity of the health care system, the lack of language interpreters at medical centers, and the absence of transportation. In addition, there are other barriers, such as the fear of being deported, mistrust of the health care system that justifiably follows ongoing discrimination and mistreatment, and a history of medical experimentation and forced sterilization.
All of these factors result in immigrant moms and babies being systematically denied affordable and accessible health care precisely when their immediate and long-term health requires it. This is unacceptable and must be remedied.
Immigration Policy Threatens the Health of Immigrant Moms and Babies
Living in the United States in itself can be toxic for immigrants. Given that immigrants are predominantly Black, Indigenous, or other people of color, they bear the brunt not only of xenophobia, but also of systemic racism in the United States. In addition, factors such as race, gender, language proficiency, country of origin, occupation, immigrant status, and duration of stay interact in complex ways that are not well explored due to the lack of disaggregated data. Unless immigration policy pays attention to these intersecting experiences, immigrant moms and babies will continue to be harmed, and their health will suffer.
- ICE detained more than 4,600 pregnant women between 2016 and 2018,14and 28 of those women reported miscarriages between 2017 and 2018. Many miscarriages were attributed to inadequate and delayed medical attention, the denial of prenatal care, and being subjected to practices such as shackling around the abdomen. There were also news reports of immigrant women being forcibly sterilized in 2020.
- Based on a study in Iowa, infants born to Latina** mothers after an immigration raid were at a 24 percent greater risk of low birth weight, regardless of the mother’s citizenship and country of origin.
- When Oregon extended health insurance coverage to undocumented mothers, they received an average of seven more doctor visits, the rate of screening for gestational diabetes increased by 61 percent, and the number who received at least one fetal ultrasound increased by 74 percent. This improved level of care led to a decrease in rates of low birth weight and child mortality.
- Undocumented mothers are more likely to experience pregnancy complications including excessive bleeding and fetal distress, postpartum depression, and unplanned caesarean sections.
- Even though foreign-born Latina mothers have better birth outcomes compared to other mothers, this “immigrant advantage” diminishes the longer they live in the United States.
Recommendations:
- Congress must pass the HEAL for Immigrant Women and Families Act to expand immigrants’ eligibility for health insurance coverage and access to care, including maternity and infant care and sexual and reproductive health services.
- Congress must pass the Health Equity and Accountability Act to address health care disparities affecting communities of color, rural communities, and other underserved populations, through the promotion of culturally appropriate care, data collection, and reporting.
- Congressional appropriators should increase investments in community-based maternal health solutions and safety-net programs such as Title X and Community Health Centers that provide crucial health care to immigrants.
- The U.S. Department of Health and Human Services (HHS) should rescind the Trump Administration’s harmful changes to regulations, executing Section 1557 of the Patient Protection and Affordable Care Act, also known as the Health Care Rights Law. HHS should instead strengthen protections against discrimination in health care.
- Congress must pass the Protecting Sensitive Locations Act, which prohibits immigration enforcement actions within 1,000 feet of a “sensitive location” such as health care facilities, schools, or places of worship.
- Congress must pass legislation to improve disaggregated maternal health data collection, including the Data to Save Moms Act (H.R. 925 / S. 347), the Maternal Health Pandemic Response Act (both part of the Black Maternal Health Momnibus), the MOMMA’s Act (S. 411), and the Quality Care for Moms and Babies Act.
- Congress must pass the Border Zone Reasonableness Restoration Act, which would limit the “border zone” immigration enforcement and search-and-seizure activities of the Department of Homeland Security. The current 100-mile border enforcement zone chills and impedes immigrants’ ability to participate fully in community life, including seeking health care.
* We recognize and respect that pregnant, birthing, postpartum, and parenting people have a range of gender identities, and do not always identify as “women” or “mothers.” In recognition of the diversity of identities, this series prioritizes the use of non-gendered language where possible.
** To be more inclusive of diverse gender identities, this bulletin uses “Latinx” to describe people who trace their roots to Latin America, except where the research uses Latino/a and Hispanic, to ensure fidelity to the data.

