The Mercy Birthing Center illustrates the potential of a nourishing midwifery-led unit within a hospital. The center is a separate unit operated by CNMs within Mercy Hospital St. Louis. It was established in response to women’s growing interests in receiving support for physiologic childbearing.
The homelike center includes four birthing suites with tubs and showers, a central living room and kitchen, an area for classes, and rooms for prenatal and postpartum and newborn visits. The center offers comfort measures as well as nitrous oxide (“laughing gas”) to help women cope with labor. The midwives use handheld devices for monitoring the fetal heart status (“intermittent auscultation”). In contrast to many typical hospital settings, laboring women are free to eat, drink, and move about, according to their interest, and to give birth in their position of choice. If they need higher levels of care (for example, an epidural or continuous electronic fetal monitoring) or develop a complication or concern, their midwife can accompany them upstairs to the standard labor unit and continue to care for them there. Care by obstetricians and maternal-fetal medicine specialists is available if needed.
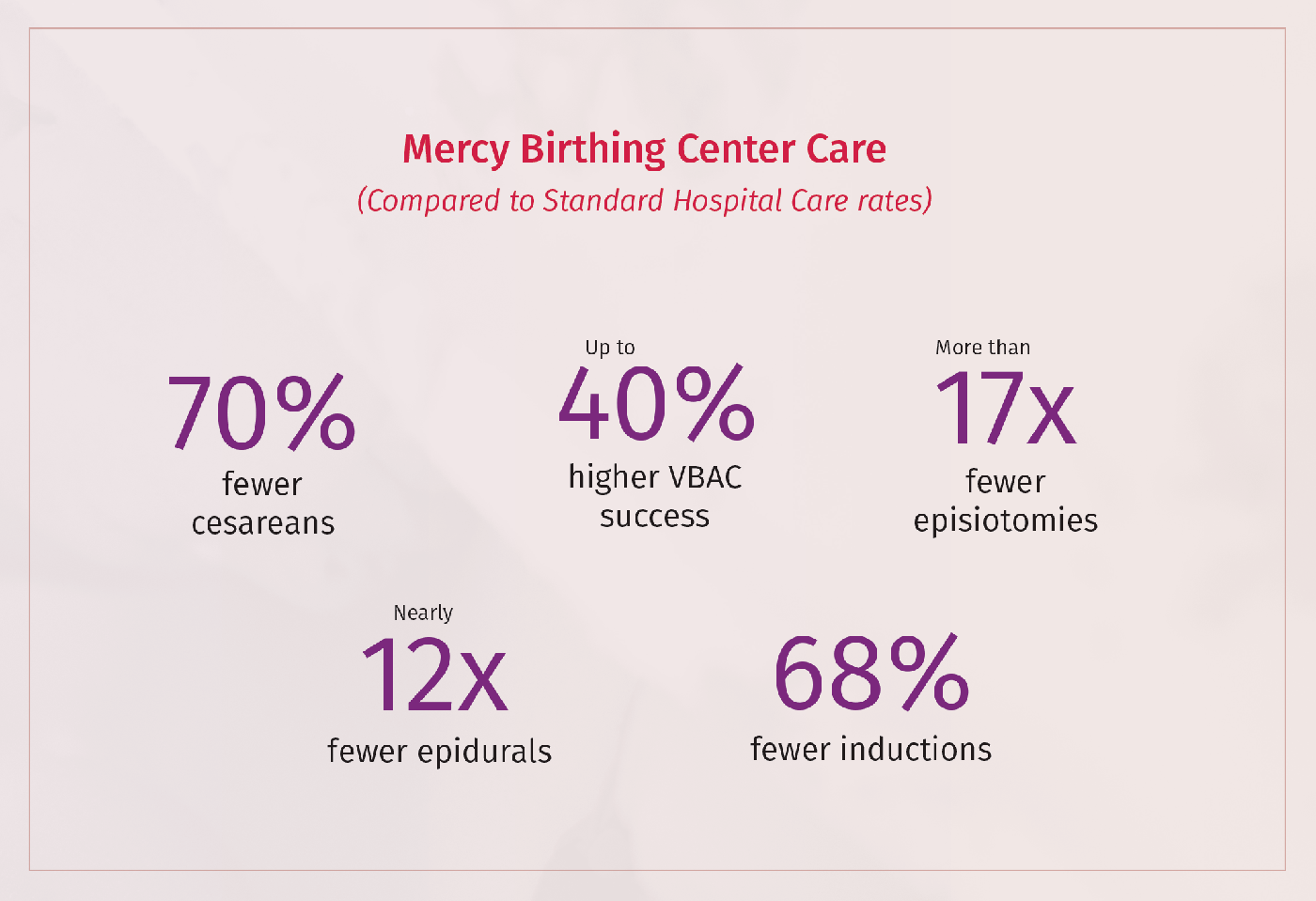
The center’s care and outcomes contrast sharply with standard hospital birthing care:
- Their cesarean rate is 70 percent lower than that national average (less than one out of 10 births, compared to one in three).
- Their rate of vaginal births after a cesarean (VBAC) among women planning to have one is up to 40 percent higher (84 percent compared to usual rates of 60 to 80 percent, depending on the study).
- Their episiotomy rate is only 0.4 percent, compared to 6.9 percent among hospitals reporting in 2018 — more than 17 times higher.
- Their epidural rate was 6.4 percent, versus 75 percent nationally in 2019.
- Their labor induction rate (8.7 percent) was 68 percent lower than national rates reported on 2019 birth certificates. However, birth certificates are known to greatly undercount inductions. For example, women in California who gave birth in 2016 reported a rate of 40 percent.
In addition to these excellent clinical outcomes, 100 percent of their clients reported they would recommend this care to friends.
Eligible lower-risk women with Medicaid or private insurance typically have coverage for prenatal, hospital birth, and postpartum and care with CNMs. Thus, when cost sharing is not onerous, financial barriers to access at the Mercy Birthing Center are minimal. However, very few hospitals offer comparable midwifery-led units.

